
Prior to gaining departmental status, Radiation Oncology was a division of the Department of Radiology within the Mallinckrodt Institute of Radiology. Radiation Oncology services have a long and rich history at Washington University. With the opening of the Edward Mallinckrodt Institute of Radiology on February 28, 1931, Sherwood Moore, MD, served as director for the Department of Radiology, with four radiologists and one physicist on staff. The ground floor of the nine-story building was devoted to radiation therapy and a small film library.
In 1951, MIR’s second director, Hugh Wilson, MD, established a radiation therapy section – a groundbreaking move, since radiation therapy as a separate modality was a relatively new concept in the medical community. Dr. Wilson recruited William Moss, MD, to head the newly established section. At the time, Dr. Moss was the only physician practicing radiation therapy in the St. Louis area. Dr. Moss left a few years later, and William Seaman, MD, took charge until his departure in 1956. William Powers, MD, succeeded Dr. Seaman. Dr. Powers was responsible for simulators, linear accelerators and treatment planning.
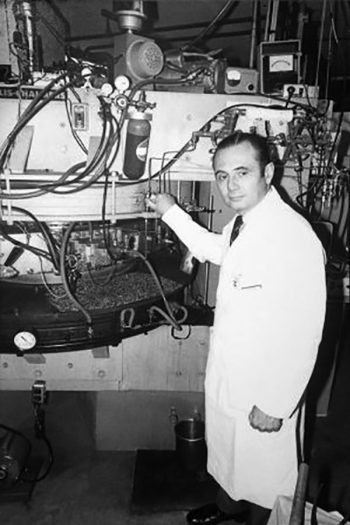
The cyclotron played a pivotal role in the history of radiology and radiation therapy. In the late 1950s, William Powers, MD, the first director of Radiation Therapy, and Mallinckrodt Institute physicist
Michel Ter-Pogossian, PhD, conducted successful research using cyclotron-produced radioactive oxygen to study the distribution of oxygen in malignant tumors.
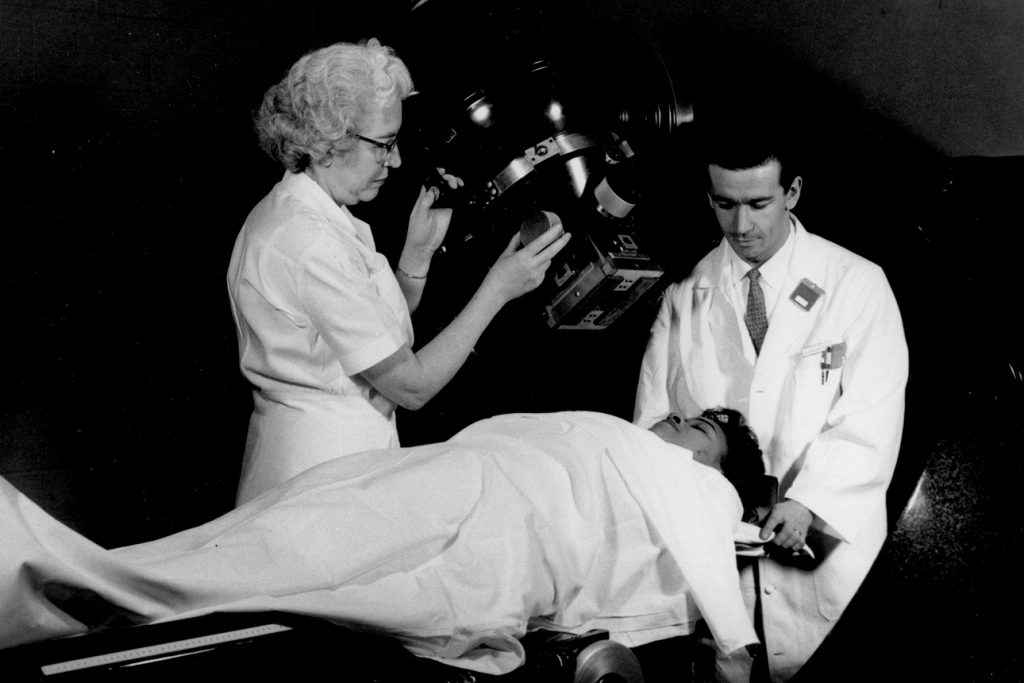
In 1963, MIR added a Picker Cobalt 60, one of the country’s first high-energy LINAC units used to treat cancers, especially of the head and neck.

William Powers, MD, developed a custom-shaped form using the alloy Cerrobend to block the delivery of radiation to any area outside the treatment site. The Cerrobend blocking system was the forerunner of conformal radiation therapy.
Carlos Perez, MD, initiates a program for the training of radiation therapy technologists. This program, the first of its kind in the United States, becomes nationally recognized for its standard of excellence.
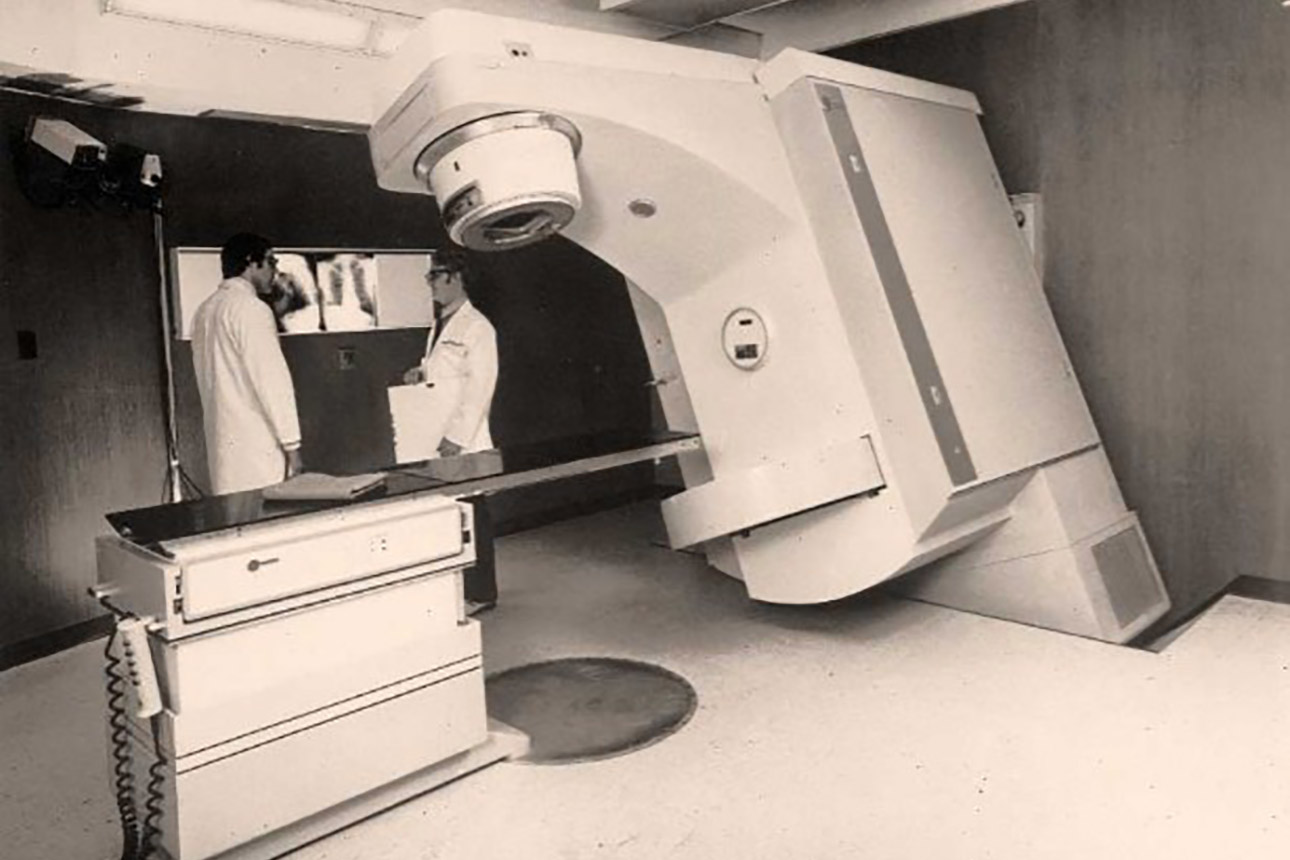
Radiation therapy faculty collaborated with Varian Associates in developing the first generation of dual-modality, high-energy linear accelerators. The Clinac 35 was the first accelerator with a built-in computer and the capability to produce short-lived radioactive isotopes.
A pioneering team of physical chemists, chemists, and physicians led by Michel Ter-Pogossian, PhD, develop positron-emission tomography (PET).
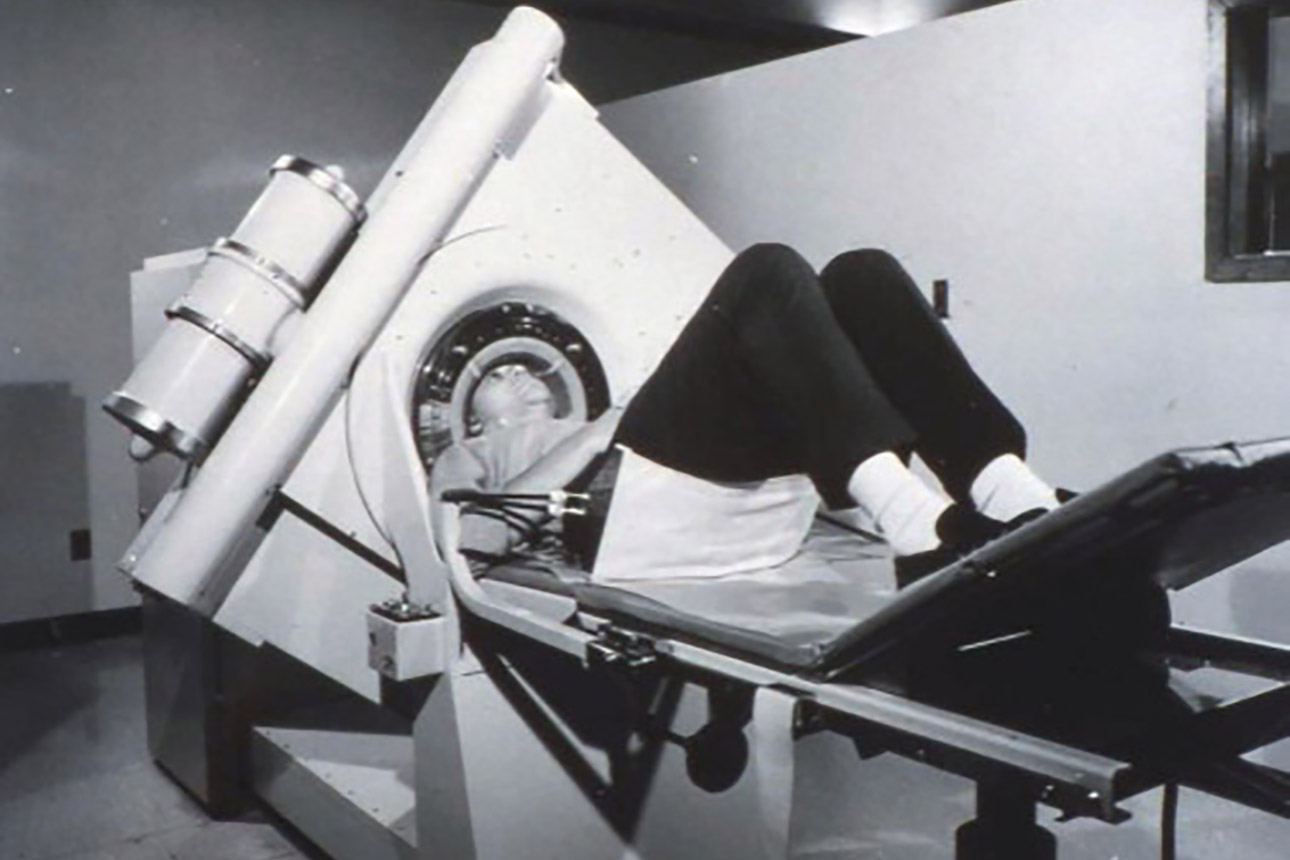
Mallinckrodt Institute of Radiology becomes a partner of London-based EMI Ltd. in developing CT scanning. One of EMI’s first two prototype CT units capable of imaging the entire body is installed at MIR the next year.
The Cancer Information Center opens. The first of its kind in the United States, it becomes a model for other centers, serving 877 patients in its first year.

Cancer Biology scientists, led by Joseph Roti Roti, PhD, developed a new technique for simplifying the identification of hormone-responsive tumors and improving the reliability of assay procedures.
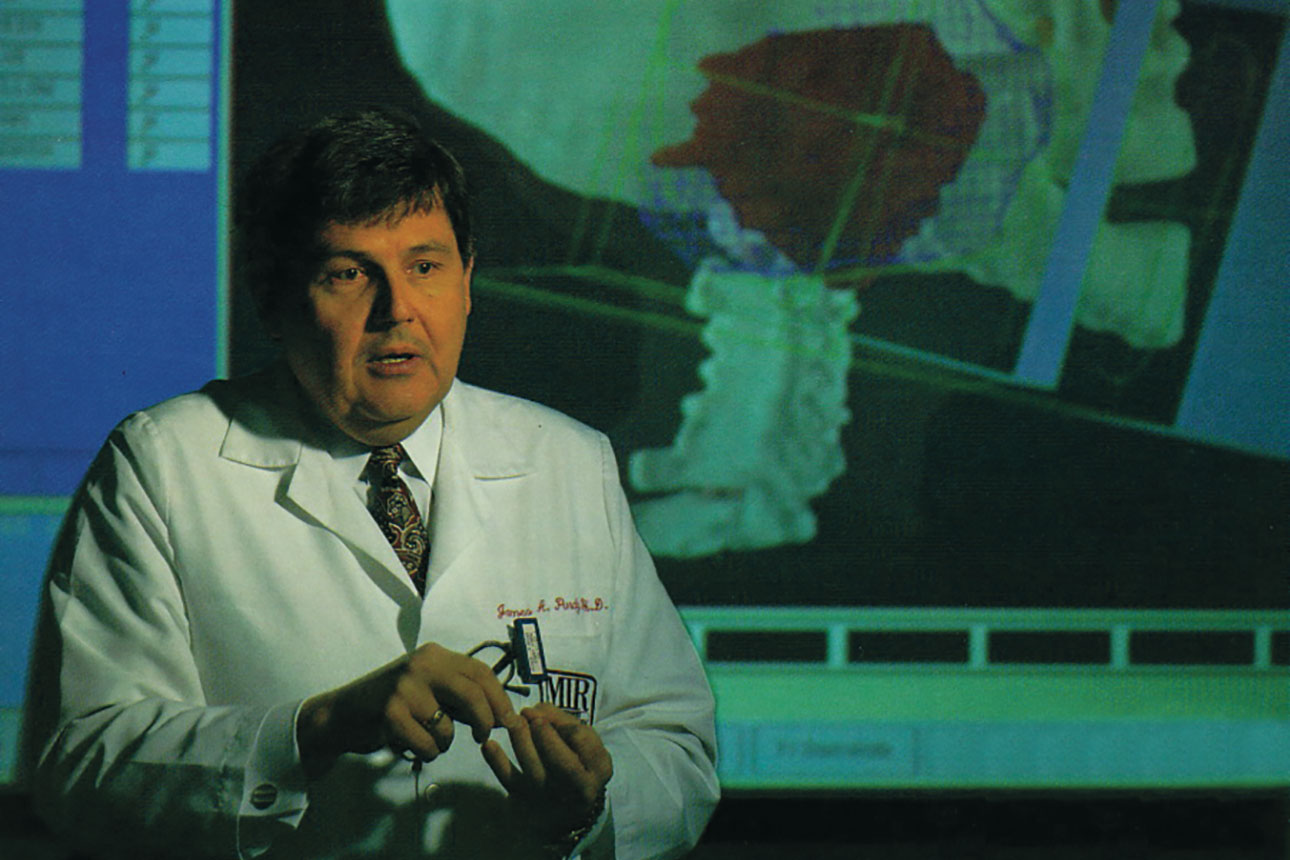
Radiation oncology physicists, led by James Purdy, PhD, developed a 3-D treatment planning system for cancer. In 1991, the Radiation Oncology Center opened the St. Louis area’s first 3-D treatment planning center, using a CT scanner equipped with a laser-marking system and connected to a computer that targeted hard-to-treat cancer sites.
The Washington University Medical Physics Residency Program becomes the first of its kind to be accredited by the Commission on Accreditation of Medical Physics Education Programs (CAMPEP).
Learn more about Medical Physics Residency at Washington University School of Medicine »

Gamma Knife stereotactic radiosurgery has been in use at Washington University Medical Center since 1998. The technology uses gamma rays produced by a Cobalt-60 source to precisely target and destroy abnormalities with the brain. This service has been a highly successful collaboration between Radiation Oncology and the Department of Neurosurgery.

Washington University Radiation Oncology is instrumental in developing the world’s first big bore CT scanner, featuring an 85cm bore to allow for better positioning and imaging for patients with immobilization devices. Today it is the de facto standard for real time simulation and CT imaging.
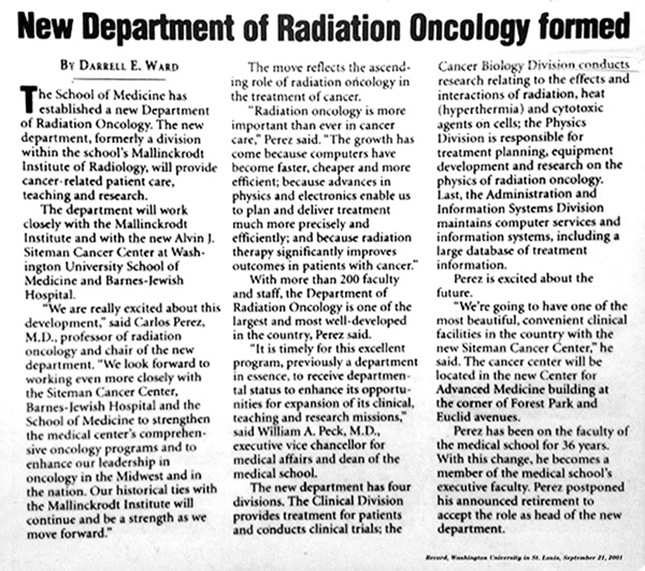
The Department of Radiation Oncology was established to address institutional goals. Prior to this, the department was a division of the Department of Radiology. The Siteman Cancer Center was established in 1999, and in 2001 became an National Cancer Institute (NCI)-designated cancer center. It was designated a Comprehensive Cancer Center by the NCI in 2005. At that time, nearly all NCI comprehensive cancer centers had Radiation Oncology Departments, and radiation oncologists on cancer center leadership committees. William A Peck, MD, executive vice chancellor for medical affairs and dean of the medical school stated, “It is timely for this excellent program, previously a department in essence, to receive departmental status to enhance its opportunities for expansion of its clinical, teaching and research missions.” Departmental status was also needed to recruit a national leader in Radiation Oncology. At the time, the newly formed department had 35 faculty including 10 radiation oncologists.
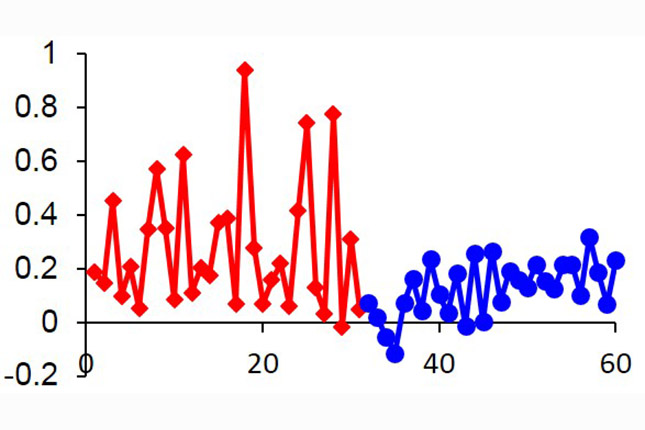
Reduced plan variability is demonstrated by using knowledge based planning, developed by medical physicists from the Department of Radiation Oncology.
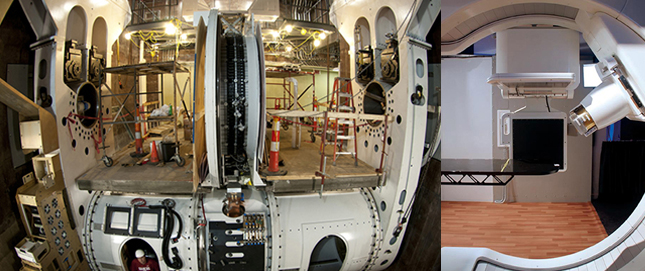
On December 18, 2013, the first patient treatment on the world’s first compact proton therapy system is performed at the S. Lee Kling Center for Proton Therapy.

On January 15, 2014, the world’s first MRI-Guided Radiation Therapy treatment is performed at Washington University School of Medicine. The ViewRay machine used to perform this treatment was developed by James Dempsey, PhD, who completed his doctoral and postdoctoral studies, as well as his medical physics residency, in the Department of Radiation Oncology at Washington University School of Medicine.
In March, 2017, all of the Washington University in St. Louis/Barnes-Jewish Hospital Radiation Oncology facilities (Alton Memorial Hospital, Barnes-Jewish Hospital and South County, Barnes-Jewish St. Peters Hospital, Barnes-Jewish West County Hospital, and Christian Hospital) achieved accreditation from the American Society for Radiation Oncology (ASTRO) Accreditation Program for Excellence (APEx), which last for four years. The unilateral success of all six facilities was the result of a multi-year effort to standardize procedures and quality of care, to allow patient portability and service coordination, and to enable sharing of resources, staff and expertise across all involved institutions.