Tell me about your background.
In 2012, I received my Bachelors of Science in Kinesiology and Sports Medicine from the University of Virginia. After working as a physical therapy technician for two years, I decided to go back to school and complete a Masters of Science in Health and Movement Sciences at Virginia Commonwealth University (2016) and a PhD in Rehabilitation and Movement Sciences at the same institution (2021). At VCU, my research focused on the peripheral vascular inflammatory responses to exercise, physical activity, and diet. After defending my dissertation in June of 2021, I began working as a Postdoctoral Research Associate in Dr. Carmen Bergom’s Translational Radiation Cardiobiology Lab here at WUSM.
What led you to study at Washington University?
During my PhD, we conducted multiple clinical trials investigating how changes in physical activity and diet could impact cardiometabolic health in survivors of breast cancer and in patients undergoing treatment for non-Hodgkin’s lymphoma. These studies led me to have a specific research interest in the mechanisms underlying cancer treatment-induced cardiotoxicity. The primary focus of the Bergom Lab here at WUSM is to use pre-clinical models to investigate the genetic and cellular mechanisms underlying radiation-induced cardiac dysfunction, and so I knew that conducting my postdoctoral research with Dr. Bergom would be an amazing opportunity to both further my research interests and to receive world-class training/mentorship.
What are your future career goals?
My ultimate goal is to lead a well-funded laboratory whose research determines how lifestyle changes – such as exercise, physical activity, and diet – alter the cellular mechanisms underlying cancer treatment-induced cardiac dysfunction. More specifically, I hope to become a leader in the field of cancer treatment-induced cardiac inflammation.
What are you working on right now?
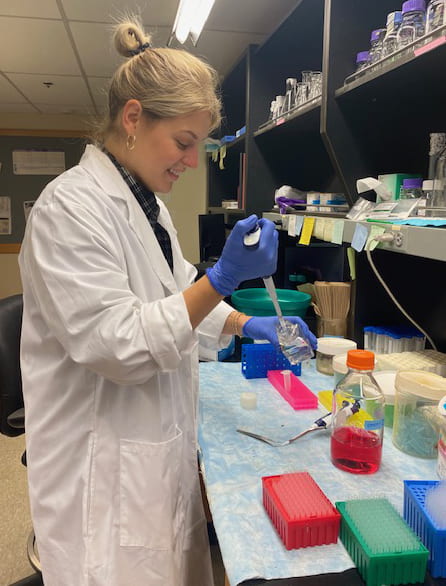
The Bergom Lab is conducting so many exciting projects right now! The goal of my independent project is to determine how cardiac macrophage populations contribute to radiation-induced cardiac dysfunction (RICD), however we are also investigating genetic modifiers of RICD, the impact of intermittent fasting on RICD, and how low-dose radiation affects cardiac remodeling in the setting of heart failure.
What has been the most challenging aspect of this specific area of study?
As a trainee with little background in radiobiology, it has been challenging to understand the complexities of radiation planning/delivery and to try to implement radiation plans in our preclinical models that recapitulate the toxicities observed in human patients.
What are your future plans for this subject?
We are continuing to work on the projects I touched on above, in hopes of identifying a cellular/genetic mechanisms that could be therapeutically targeted to prevent RICD and/or to improve cardiovascular care in thoracic cancer patients receiving radiation.
Was there something in particular that led you to this subject of research?
In general, cancer treatment-induced cardiotoxicity is an exciting field because of the number of cancer survivors whose lives can be improved by our research. Modern cancer treatments are improving survival for many patients, yet cancer treatment-induced toxicities can limit their quality of life down the road. Our hope is to help combat that by determining how radiation and other cancer treatments impact the heart and if we can improve how these toxicities are detected, prevented, and/or treated.
In terms of my independent project, my graduate research focused specifically on the responses of peripheral vascular macrophages to exercise, physical activity, and diet. These cells, and others of the innate immune system, are fascinating in that they are extremely plastic both in phenotype and function. They are abundant in the heart and have been found to be critical to heart repair after ischemic injury, so I am really interested to see how macrophage biology contributes to radiation injury in the heart.
How did your invited talk at RRS come about? Tell us about your experience as a trainee presenting at RRS.
I am so grateful to have been given the opportunity to discuss our work at RRS! It was an honor to speak amongst panelists who are leaders in the fields of radiobiology and radiation cardiotoxicity. I felt that my invited talk was well-received and opened up a few interesting opportunities for collaboration with other RRS members.
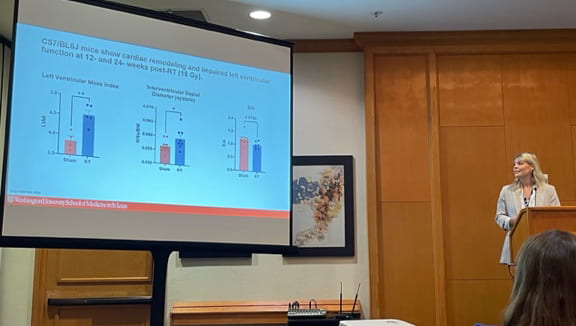
RRS 2022 was my first in-person RRS meeting, and it certainly lived up to the high praise of my colleagues – so many excellent sessions and networking opportunities and, of course, Hawaii was a beautiful backdrop! The SIT Workshop was also a great opportunity to meet and network with other trainees. I’m certainly looking forward to future meetings.
Any other comments or advice to other prospective scientists?
My only advice to other prospective scientists, especially trainees, is to not be afraid to do research outside of your “comfort zone.” Having transitioned from a very applied, exercise physiology graduate background into a postdoc focused more on basic biology and immunology research, I’ve appreciated how the transition has allowed me to grow as a researcher. I’ve found that my colleagues here at WUSM are extremely welcoming of my perspectives and are also generous with their time/resources to help me learn.
Lauren is a member of the Carmen Bergom Lab.